Ehlers-Danlos syndrome
I thought it would be useful to post my letter from the consultant diagnosing my EDS, as so many people have asked me to comment on my diagnosis.
Many thanks for suggesting that I might see this 29-year old former nursing axillary who started nursing studies in 2007 but was forced to take off her second year of study because of her illness. I note that she has suffered from abdominal pain since birth. Currently she suffers from constipation and bloating and severe weight loss. She has an eight-year old daughter and a six year old son, both of whom like her are hypermobile as is her mother and was her late maternal grandmother. Like many hypermobile people she walked late at 16 months and bottom shuffled as an alternative to crawling prior to this. As a child she W-sat, performed contortionist tricks and was noted to be bendy and clumsy. She tended to twist her ankles and strain her wrists playing tennis. In her teens she developed so-called growing pains in her knees. For the past 5 years she has experienced pain in her knees on standing and in her hands on typing or opening jars. She also has intermittent neck pain which radiates to her shoulders and occasional lower back pain on lifting. She has experienced right sided sciatica during pregnancy. Compatible with a hypermobility syndrome are the wide spread joint clicking, easy bruising, poor skin healing, resistance to local anaesthetics at the dentist and orthostatic intolerance over the last six years with three attacks of presyncope. Since March 2010, the pain has become life dominating and associated with fatigue.
My examination confirmed the presence of widespread joint laxity with a hypermobility score of 6/9 on the hypermobility scale. Outside the scale her cervical spine, small finger and toe joints were also affected, as were her feet which flattened and pronated on weight-bearing. There was a 4 degree scoliosis on the Burnell scoliometer but no other features of a marfanoid habitus. Her skin showed increased stretchiness in the phase of taking up slack. There were no striae atrophicae but striae gradivarum were very marked. Gorlin sign (the ability to touch the nose with the tip of the tongue) was negative. The lingual frenulum was present (normal).
On the basis of two major and one minor criteria she satisfies the 1998 Brighton criteria for the joint hypermobility syndrome, equivalent to the Ehlers-Danlos syndrome hypermobility type formerly EDS III. I explained the nature of the condition to her, in particular its genetic basis and the vulnerability it confers on soft tissues to the effects of injury and overuse. In her case it has resulted in long standing joint and spinal pain. It may well provide a rational basis for her long standing abdominal symptoms.
I look forward to hearing the outcome of your investigations in due course. I have reffered her to our team of specialist physiotherapists in hypermobility at the hospital here for an assessment and appropriate course of treatment as appropriate.
I am happy to review her from time to time as and when the need arises.
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
Here is a great article I found explaining EDS/ Hypermobility.
Pain & the Hypermobility Syndrome
RODNEY GRAHAME CBE, MD, FRCP, FACP
Emeritus Professor of Rheumatology, University College Hospital, LONDON.
Emeritus Professor of Rheumatology, University College Hospital, LONDON.
When the Hypermobility Syndrome was first put on the medical map in 1967, it was defined as the presence of musculoskeletal symptoms (predominantly pain) occurring in otherwise healthy individuals. Thirty years down the line we now think that there are probably two types of hypermobility.
The first is a milder type occurring in people whose joints are just like everyone else's but which have the capacity to move more than most people's joints. The other, a more marked form, has features that suggest that it may be part of an inherited connective tissue disorder similar to the hypermobile form of the Ehlers-Danlos Syndrome, formerly called EDS III. It probably is EDS. At the present time we simply do not know for certain whether or not HMS is merely a less severe type of EDS III. Pain can occur in other forms. For the rest of this article, in order to avoid confusion, I will refer to it as one condition, the HMS/EDS. There are many people with joint hypermobility in the community who experience no (or very little) pain. Most of them probably do not even know that they are hypermobile at all. Then something happens, and they start getting pains for the first time in their lives. Usually unexpected exercise or a change of job or lifestyle provokes the onset of pain. When ever symptoms commence, and irrespective of the cause of the hypermobility, the term 'Hypermobility Syndrome' is used to describe the condition. Hypermobile people without pain are just called hypermobile people.
A little known fact is that hypermobility occurs in many individuals in a few joints only. It does not necessarily have to affect all one's joints. Even hypermobility in a single joint can cause pain and/or instability in that joint; the diagnosis is still Hypermobility Syndrome (HMS/EDS).
People are born hypermobile. It is in their genes. It is the way they are made. So how is it that people with hypermobility can be literally fine for decades, only to be laid low from widespread pain, often out of the blue, which may make its unwelcome appearance during childhood, adolescence, or adult life? To explain these curious and seemingly inexplicable happenings, we postulate that the affected person, in this case the hypermobile person, had an inbuilt weakness of her (it is usually a 'her' but not always) strength-providing collagen or similar protein. This weakness renders body tissues less robust and hence less able to stand up to the physical strains of everyday life. We can explain a lot of the pain that arises on the basis of a series of (often quite minor) injuries that occur whenever there is a mismatch between the physical demands on one hand, and the strength of the parts being asked to perform them on the other. There is a whole host of painful injuries that can result, ranging from dislocations to fractures, disc prolapse, ligament sprains, muscle strains, pulled tendons (like tennis elbow or plantar fasciitis), etc.- conditions that can happen to anyone, but which occur more easily in those with the HMS/EDS. If one only knew one's strength (or lack of it), one should be able, in theory at least, to stay within the safety margin and thereby protect oneself from injury. Up to a point this is so. Many people with the HMS/EDS are able to modify their lifestyle and do just that. Others find it more difficult.
A joint that is beginning to wear starts to lose its cartilage or gristle, which is essential for the smooth movement between the adjoining bones. This wear heralds the onset of osteoarthritis, a condition painful in its own right. It is a very common form of arthritis in middle and old age, and one to which hypermobile people seem to be prone, in many cases at an early age. It is important to establish as far as possible to what extent the pain is due to trauma/overuse or to early onset osteoarthritis, as the treatment is very different. The emphasis with the former is on prevention, while with the latter it is on treatment by one form or another.
However, neither susceptibility to injury or overuse (repetitive injury), nor osteoarthritis, explains all the pain that is felt in the HMS/EDS. There is more to it than that.
"Emotional influences can amplify pain, but they do not cause it." |
Let us try to piece the jigsaw together. Pain is something we feel. Even if it has a physical cause, as it undoubtedly has in the HMS/EDS, it is still a subjective experience. It is often accompanied by an intense sense of exhaustion. the severity of the pain we feel is greatly influenced by our state of mind. If we are upset or agitated it tends to increase. If we are content, relaxed or just happy it tends to diminish. The HMS/EDS people are often in the former category, and for good reason! Lack of understanding of the condition is widespread, and this, coupled with failure to receive adequate treatment for relief of symptoms, leads to frustration, resentment, anger (and lots more emotions which I could list but readers know them all only too well!) and, ultimately depression. These emotional influences can amplify pain, but they do not cause it.
Another piece of the jigsaw is a mysterious condition called fibromyalgia. This condition causes widespread chronic pain in muscles and is identified by the finding of multiple 'tender points' at specific sites in the body. For years the debate has raged as to whether it is a physical disease affecting the muscles, or whether it is an emotional disorder. The prevailing view is that it is probably some form of distress signal that can arise in people with a number of different and unrelated conditions. How this relates to hypermobility is that it has been shown that hypermobility and fibromyalgia occur together in the same person more often than one would expect on the basis of a chance happening. It does not mean that they are part of the same condition. It would, indeed be very unlikely that what is clearly an acquired disorder (fibromyalgia) could be an integral part of what is clearly a genetic one (HMS/EDS). More likely, the fibromyalgia should be regarded as a signal emanating from a distressed HMS/EDS person. But fibromyalgia occurs only uncommonly in the HMS/EDS. We must look further afield.
It seems quite likely that there may be a totally different explanation for the burden of pain borne by people with the HMS/EDS. Here are two clues:
The first clue relates to the sense called proprioception, which means knowing where parts of one's body are in space. If you close your eyes and somebody bends your finger for you or picks your arm up, you know immediately how far your finger is bent or where your arm now is. That is because you have good proprioception. Scientists have shown that people with the HMS/EDS are not quite as good as other people in knowing exactly where their fingers or arms etc are in space. This could lead to a further increase in the risk of injury.
The second clue is the discovery that patients with the HMS/EDS for some reason do not appear to experience the full anaesthetic affect of lignocaine injections when these are given for dental purposes, minor surgery or for epidural anaesthesia (I wonder how many readers are nodding their heads as they read this!).
At the present time we do not know quite what either of these clues means or whether they relate to one another. But they do suggest that people with the HMS/EDS, in addition to their proneness to injury, dislocation and osteoarthritis, may also have a fault in the way their pain signals are picked up for onward transmission to the brain, where they reach conciousness. Research work is in progress to try to sort out this enigma. Much more needs to be done. Watch this space!
Readers will know that many conventional methods of treatment, of the kind offered for rheumatic complaints in general, are not particularly helpful in the HMS/EDS. Physiotherapy still carries the best prospect for pain relief, and it is encouraging that more physiotherapists are training in methods that are helpful in this condition. Another noteworthy development is the network of units throughout the country that are offering pain management programmes, an approach which has been shown to be beneficial in the HMS/EDS where intractable pain is present.
Revised 15 March 2009
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
This is from the current DWP disability hand book, for anyone struggling to explain, you don't have to...just point their own guidelines out to them!
6.6 Joint Hypermobility Syndrome
6.6.1 The Joint Hypermobility Syndrome (JHS) is a multi-system inherited connective tissue disorder thought to be caused by faulty fibrous tissue matrix proteins such as collagen. It is indistinguishable from Ehlers-Danlos Syndrome – Hypermobility type (previously known as Ehlers-Danlos type III).6.6.2 Tissue laxity results in increased flexibility, an asset to some dancers, gymnasts, musicians and athletes. However, fragile tissues are prone to overuse injury, rupture and healing is poor and often delayed.
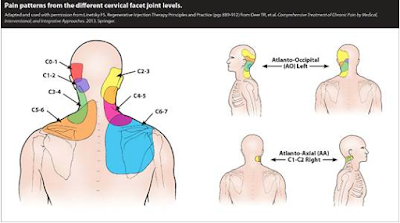
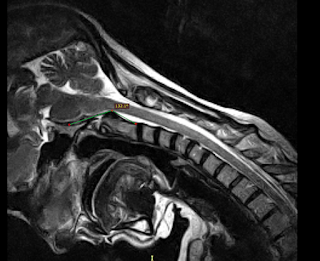
Muscle and joint complications - joint pain, sprains, tendonitis, bursitis, recurrent dislocations, fractures, early arthritis and osteoporosis, chronic spinal disc problems with back and neck pain, chronic pain syndrome.
Other complications - stretchy poor healing skin, uterine and rectal prolapse and stress incontinence, proprioceptive impairment leading to clumsiness and falls, fatigue. Gastro-intestinal problems (abdominal pain, constipation, gastroparesis, reflux – can require multiple medications and even naso-gastric tube or PEG feeding). Autonomic Disorders occur in 78% of patients and include Vasodepressor Syncope and Postural Orthostatic Tachycardia Syndrome (PoTS) (increased pulse rate on standing or prolonged sitting can result in reduced blood supply to the brain and compensatory high adrenaline levels. Symptoms include fainting, dizziness, fatigue, poor concentration and memory problems, headaches, palpitations, tremor, sense of anxiety, nausea, sweats and visual problems. It produces functional impairment similar to that found in COPD and heart failure).
6.6.3 Joint Hypermobility Syndrome is under-diagnosed. In one survey, over 50% of patients waited over 10 years from onset of symptoms to receive a diagnosis. Many doctors (including some rheumatologists) are sceptical about its serious impact on patient’s lives.
It can be difficult to match disability with patient appearance as they often look and move well .Assessors may incorrectly assume that because a joint has good range of movement and is not swollen, it cannot be painful.
6.6.4 People with JHS often respond poorly to analgesics and local anaesthetics. With frequent and persistent painful episodes and poor pain control, they often develop widespread chronic pain with pain amplification and kinesiophobia (avoidance of movement to avoid pain). Deconditioning develops.
Depression is common due to chronic uncontrolled pain, difficulty with tasks of daily living, diagnostic delay and failure to recognise symptom severity.
6.6.5 Care Needs
(i) People with severe forms of the Joint Hypermobility Syndrome may be in frequent or constant pain that is worsened by movements, especially those involving physical effort such as lifting. Joints may dislocate following minimal movement. When the tissues are damaged, physically demanding activities are also painful and give rise to care needs from another person. Periods of rest throughout the day may be required after only a modest amount of physical activity. Falls may occur so that certain activities such as bathing,
using stairs, etc may need to be supervised, particularly in elderly people with this syndrome.
(ii) Main meal preparation, especially cutting up vegetables, opening jars, lifting pans and using taps may prove to be difficult .At times assistance may be required with toileting and personal hygiene.
(iii) Special consideration may be required in the workplace. Chairs may need to be adapted to suit individual’s need e.g. high back, lumbar support, elevated seat. It may be necessary to adapt taps and door-handles. Repetitive use of susceptible joints should be avoided. Special transport considerations may be necessary. Advice from an occupational therapist, physiotherapist or occupational health department may be helpful. Employees with autonomic complications may require a cool environment with the ability to take short regular breaks to eat and drink. Prolonged standing and sitting should be avoided. They may have special dietary requirements. Profound fatigue is a common problem and can impair stamina and concentration.
6.6.6 Mobility Considerations
(i) Because the connective tissues are lax and fragile they may be easily injured or dislocate. The combination of unstable, painful joints and balance problems may make walking difficult. People with severe forms of the syndrome require the use of walking aids (cane, crutches) or wheelchair. Patients can become bed-bound.
6.6.7 Duration of Needs
(i) Pain can result from sudden injuries to the soft tissues which take weeks or months to heal. Overenthusiastic physiotherapy from practitioners inexperienced with Joint Hypermobility Syndrome may exacerbate symptoms. Long delays in diagnosis means that many patients (for example 24 % of patient attending their first appointment at UCH Hypermobility Clinic) have established chronic pain syndrome and requiring a multi-disciplinary team approach to management.
6.7 Further Evidence
Because of the wide range of clinical manifestations and spectrum of disability and needs it may often be necessary to obtain further evidence, in the form of a GP or physiotherapist report or a report by an examining medical practitioner. A rheumatologist’s report may be particularly helpful.
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
This is from the current DWP disability hand book, for anyone struggling to explain, you don't have to...just point their own guidelines out to them!
6.6 Joint Hypermobility Syndrome
6.6.1 The Joint Hypermobility Syndrome (JHS) is a multi-system inherited connective tissue disorder thought to be caused by faulty fibrous tissue matrix proteins such as collagen. It is indistinguishable from Ehlers-Danlos Syndrome – Hypermobility type (previously known as Ehlers-Danlos type III).6.6.2 Tissue laxity results in increased flexibility, an asset to some dancers, gymnasts, musicians and athletes. However, fragile tissues are prone to overuse injury, rupture and healing is poor and often delayed.
Muscle and joint complications - joint pain, sprains, tendonitis, bursitis, recurrent dislocations, fractures, early arthritis and osteoporosis, chronic spinal disc problems with back and neck pain, chronic pain syndrome.
Other complications - stretchy poor healing skin, uterine and rectal prolapse and stress incontinence, proprioceptive impairment leading to clumsiness and falls, fatigue. Gastro-intestinal problems (abdominal pain, constipation, gastroparesis, reflux – can require multiple medications and even naso-gastric tube or PEG feeding). Autonomic Disorders occur in 78% of patients and include Vasodepressor Syncope and Postural Orthostatic Tachycardia Syndrome (PoTS) (increased pulse rate on standing or prolonged sitting can result in reduced blood supply to the brain and compensatory high adrenaline levels. Symptoms include fainting, dizziness, fatigue, poor concentration and memory problems, headaches, palpitations, tremor, sense of anxiety, nausea, sweats and visual problems. It produces functional impairment similar to that found in COPD and heart failure).
6.6.3 Joint Hypermobility Syndrome is under-diagnosed. In one survey, over 50% of patients waited over 10 years from onset of symptoms to receive a diagnosis. Many doctors (including some rheumatologists) are sceptical about its serious impact on patient’s lives.
It can be difficult to match disability with patient appearance as they often look and move well .Assessors may incorrectly assume that because a joint has good range of movement and is not swollen, it cannot be painful.
6.6.4 People with JHS often respond poorly to analgesics and local anaesthetics. With frequent and persistent painful episodes and poor pain control, they often develop widespread chronic pain with pain amplification and kinesiophobia (avoidance of movement to avoid pain). Deconditioning develops.
Depression is common due to chronic uncontrolled pain, difficulty with tasks of daily living, diagnostic delay and failure to recognise symptom severity.
6.6.5 Care Needs
(i) People with severe forms of the Joint Hypermobility Syndrome may be in frequent or constant pain that is worsened by movements, especially those involving physical effort such as lifting. Joints may dislocate following minimal movement. When the tissues are damaged, physically demanding activities are also painful and give rise to care needs from another person. Periods of rest throughout the day may be required after only a modest amount of physical activity. Falls may occur so that certain activities such as bathing,
using stairs, etc may need to be supervised, particularly in elderly people with this syndrome.
(ii) Main meal preparation, especially cutting up vegetables, opening jars, lifting pans and using taps may prove to be difficult .At times assistance may be required with toileting and personal hygiene.
(iii) Special consideration may be required in the workplace. Chairs may need to be adapted to suit individual’s need e.g. high back, lumbar support, elevated seat. It may be necessary to adapt taps and door-handles. Repetitive use of susceptible joints should be avoided. Special transport considerations may be necessary. Advice from an occupational therapist, physiotherapist or occupational health department may be helpful. Employees with autonomic complications may require a cool environment with the ability to take short regular breaks to eat and drink. Prolonged standing and sitting should be avoided. They may have special dietary requirements. Profound fatigue is a common problem and can impair stamina and concentration.
6.6.6 Mobility Considerations
(i) Because the connective tissues are lax and fragile they may be easily injured or dislocate. The combination of unstable, painful joints and balance problems may make walking difficult. People with severe forms of the syndrome require the use of walking aids (cane, crutches) or wheelchair. Patients can become bed-bound.
6.6.7 Duration of Needs
(i) Pain can result from sudden injuries to the soft tissues which take weeks or months to heal. Overenthusiastic physiotherapy from practitioners inexperienced with Joint Hypermobility Syndrome may exacerbate symptoms. Long delays in diagnosis means that many patients (for example 24 % of patient attending their first appointment at UCH Hypermobility Clinic) have established chronic pain syndrome and requiring a multi-disciplinary team approach to management.
6.7 Further Evidence
Because of the wide range of clinical manifestations and spectrum of disability and needs it may often be necessary to obtain further evidence, in the form of a GP or physiotherapist report or a report by an examining medical practitioner. A rheumatologist’s report may be particularly helpful.
Thank you so much for posting this! This explains some of the things that I experience with EDS and confirms that those symptoms are EDS related. Isn't it great to know you are not alone in this fight?! I had to give up on becoming a PT, PTA, and a musician because of the joint pain and dislocations asociated with EDS. First I had to quit playing the guitar because it caused severe elbow, shoulder, and wrist pain. Then I could not manage the daily stresses of physical activity with being a PT or PTA. So I pursued a career in computer technology. I made it through 2 years of college for my system support tech program but was unable to continue to get my computer tech degree. I was ok with that but was never able to get a job doing what I love. In fact, I have been on disability since I was in college and approved. I have been able to minimally use my education at home but have yet to make any money with it. I pray that someday my joints and health will allow me to return to work but I am prepared for the reality that I will probably never be able to work again. :(
ReplyDeleteI just wanted to say how helpful I have found this. I had to suspend my studies at college last year, and wanted to be able to explain to them that EDS effects me much more than just having 'bendy joints.' I am hoping with the help of learning support that I might be able to complete my college course and go to University the following year, but in the mean time do not receive any sickness benefit as I struggled to know what to say to the DWP. I had to give up hairdressing as I had a wrist/hand injury that has never got better. My Rheumatologist has advised me that it likely never will, and if I returned to hairdressing this would flare up again. But I so want to be able to re-train and to be part of society once more. I think the fatigue aspect of EDS is massively undermined also, and am really interested to learn more about the condition. Thanks Again.
ReplyDeleteI am Beatrice West of 100 Adams Street, Texas, USA. I want to quickly enjoin allhere to help me say a big thanks to Doctor Uwadia Amenifo for his wonderful work he has done for my family for saving my son of his Hypermobility and scoliosis. Brethren, my son by name is called Josh, and he is 18 years old. He was very ill when he was 8 years, and was treated, we noticed that he begin to have issues with working when he was 10 years he always complain of his joints and spine, and we took him to hospital for treatment, and the doctor diagnosed hypermobility, so he was given medications, and we continued to give him his medications until when he was 15 he was also diagnosed of scoliosis in this, my son was unable to Bend forward and backward, He was Walking with pain, he Doesn’t sleep well, Wake up middle of night to toilet and During daytime he can't stand to wee wee and need to rush him to toilet. This continues for two years and I was running hectare scepter looking for how to get a cure for him. I was always doing a research online about his disease, and I found in a blog where a woman aged 50 testified of how she was cured of scoliosis by a herbal Doctor Uwadia Amenifo with the use of herbal medicine, and she didn’t have to undergo any surgery. So I found the info interesting and decided to be in contact with the said herbal doctor. In the blog were the contact details of the herbal doctor. So I pick up his contact and contacted him. After explaining what my son is going through he simply said to me that he is suffering from scoliosis that was when I then told him that also he have hypermobility. So he counseled me, and promised me that he will cure my son with his herbal medicine. So we concluded the arrangement, and he prepared the herbal medicine, and sent it to me in Texas. So I gave it to my son just as he directed and to god be the glory my son was totally cured by his herbal medicine of his hypermobility, and also hos scoliosis, and as I write this testimony, my son is totally cured and can now move well and do all he was made to do. So please I want all here to help me say a big thanks to doctor Uwadia Amenifo for his wonderful work in the life of my son. Today my son is totally cured. Please if you want to talk with doctor Uwadia Amenifo concerning your health issues, and also if you are suffering from hypermobility, and or scoliosis and you want to be cured without surgery just as my son was cured without surgery contact Dr Uwadia now on his email (doctoruwadiaamenifo@gmail.com) or call him on (+2349052015874). God bless you all.
ReplyDeleteI found this bc i have edsiii and i am having a hell of a time with intestinal problems. Specialists all think they know better but they don't know jack about eds so they brush it off. I have to become my own doctor-warrior combo... and fight for tests and scans... constantly. I appreciate knuwing it isnt just me. ❤
ReplyDelete