Gastroparesis, EDS & the Final Piece of the Jigsaw Part #3 / Cranio-cervical Instability!
I know I left Part 2 somewhat in the middle of the consultation, so I'll try and start where I left off and see where it goes. Obviously there are inevitably going to be more "parts" to this series the deeper we go, so bear with me I WILL get it all down on here eventually.
To sum up the last post in a few words, the diagnostic term for my neck issues is, Cranio-Cervical Instability. Naturally our next question was, "What can we do about it and what does it mean for the future?" This is where I struggle to explain. When it comes to brain/spinal surgery the decision process is not so cut and dry!
So, the only way to actually fix the instability in my head and neck and prevent any further neurological damage would be to fuse my skull and top two vertebrae together using metal rods (permanently immobilising my skull C1 & C2) and remove the excess tissue that is causing the brainstem compression.
Obviously this is a very risky procedure and not one to be taken lightly so we made sure to ask about alternative options (at this point I'm still trying to convince myself that it's not that bad). I went through my planned list of "alternative" treatments and therapies, from stem cell treatment and prolotherapy to physio and acupuncture but I knew by his face alone that he didn't share in my optimism. He then basically confirmed that the surgical route really is my only option, things are too advanced for that to be of benefit and could potentially cause more damage. He was very direct about it, like he knew I was trying every angle, but of course he was 5 steps ahead. I'm guessing that's down to experience!
The conversation soon switched back to surgery and a very frank discussion about my medical history. I've been dependent on TPN for my nutrition for over 5 years, in which time I've had 5 serious hospital admissions with sepsis (for those not familiar with TPN, it contains lots of sugars and fats which bacteria thrive on, so infusing tpn carries a greater risk of infection than infusing fluids or trace elements for example). My surgical history is also quite complicated and my body reacts badly to anaesthetics and pain medications often leading to lengthy admissions and additional treatments.
Based on my medical history we think the neck/head problems initially started around 2004, so he explained that we could estimate that it took roughly 5 years for gastric involvement to develop and another 8 years my neurological symptoms to get to this point (13 years in total). My overall brainstem disability index (symptoms which are a direct result of disturbance of brain activity) is currently at 50% which he told me was surprisingly good considering the extent of my problems. He was also astounded that my headache isn't constant, because obviously the level of compression never changes. Although it's quite uncharacteristic and not what he was expecting, this is a real positive and one I am truly thankful for because believe me, when the headaches do strike.... it's like no other pain on earth!!! However, 50/50 is not a helpful percentage to work with when making life and death decisions, especially when you fully understand what loosing any of the remaining 50% actually boils down to!
To break that down, this is a high risk surgery even for a fit and "healthy" person. The only reason I had to travel to Spain in the first place is because so very few Dr's worldwide actually treat CCI/AAI patients with EDS because it's so complex, so we are already on shaky ground to begin with. Having additional health issues or, "co-morbidities" then increases that risk significantly. So, if you compiled a list of all my "extra" risk factors and what we could realistically achieve in terms of symptom relief, there is no balance, just a lot of uncertainties. Dr G explained that although I do need the surgery to prevent further deterioration he wouldn't be happy to take the risk, especially with no guarantees that it would improve my gastric problems, which is my main objective. However, the risk of injury just completing simple tasks is significant enough to say that this isn't a "safe" option by any means and it's highly likely that holding off won't always be an option.
He welcomed me to go and see other experts (in the states) to ask for further opinions, but also reassured me that he wanted to keep a close eye on my case and follow up on some further investigations. Taking into account my other symptoms, he also thinks there might be areas lower down my spine that are playing a role, for lack of a better phrase, he noticed how "wonky" I am! He recommended I have some further MRI scans and send them on to him to so he can get a full picture of what's happening throughout my spine.
In the mean time our best option is to try and slow down any deterioration as much as possible. He recommended wearing a hard neck brace (philedelphia or Miami-j) to prevent my head from sliding around so much and hopefully slow down the pannus formation. It's not an ideal way forward since wearing a brace will reduce muscle tone in my neck which is crucial to supporting the head and preventing further instability but for now it's the safest option and I'm comfortable with that decision.
When we left the appointment I think we were both in a bit of shock really but I was actually feeling quite positive...relieved...justified... all those things but mostly terrified!
Here are some useful links I found whilst trying to find accurate information:
http://www.thepainrelieffoundation.com/craniocervical-instability
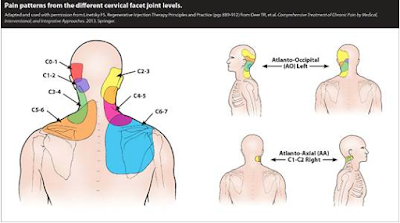
This is a great a great visual representation relating to each vertebrae in the neck which I found to be spookily close to a pain analysis image I filled in at my most recent pain management consult.
references:
http://www.instabile-halswirbelsaeule.de/angles-which-should-be-measured/
http://www.thepainrelieffoundation.com/craniocervical-instability/
https://link.springer.com/article/10.1007/s10143-017-0830-3
http://article.sciencepublishinggroup.com/html/10.11648.j.ejpm.20150304.11.html
http://doctorstock.photoshelter.com/image/I0000moMrEmEEFTE
Kanofsky Scale
Great post. I was checking continuously this blog and I am impressed!
ReplyDeleteVery helpful info specifically the ultimate phase :) I care for such information a
lot. I was looking for this certain information for a long time.
Thanks and good luck.
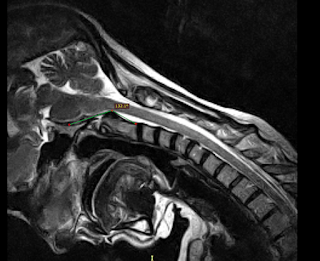
I'm having the same problems, my craniocervical junction is almost identical to yours. My CXA on my last flexion extension MRI was 131 degrees sitting. I also measured from the odontoid itself and did not include the transverse ligament or dura mater. Sitting CXA is probably closer to 127 degrees... doctors' not putting the pieces together is INCREDIBLY frustrating. Is there any way I could email you to show my measurements? I would love to speak with you because your the first person dealing with dead end after dead end. I still cant really get any doctors' to agree with me. The last guy I saw was an orthopaedic doctor. He said it was pannus which I know isn't true. It's the transverse ligament with subsequent ligaments and dura mater. The flexion image shows the spinal cord wrapping around the c2 ligaments to the point where that portion of the spinal cord is not clearly seen on the image.. Like I said, told it was pannus and he said he wouldn't do surgery but would ask the Rheumatologist to prescribe anti inflammatory pills. By the way I've dealt with doctors' for long enough to know that the Rheum appointment coming up is going to be a waste of time. The upcoming app is not an MD but a DO, not good.
ReplyDeletesorry introvert, I've only just seen a bunch of comments on here...notifications must be playing up! Was it you who sent me the email?
ReplyDeleteVery great post. I simply stumbled upon your blog and wished to say
ReplyDeletethat I have really enjoyed surfing around your weblog posts.
In any case I will be subscribing for your feed and I hope you write again very soon!