Gastroparesis, EDS, & the final piece of the jigsaw #Part 2
Click here for #Part 1
Most of you will already know through my blog, I'm not keen on surgeons (to put it mildly) so that key moment when I first meet a new one always feels like a very tense and anxious exchange. Years of plodding through the various health systems has unfortunately made me very cynical so it takes a lot to win me over these days.
... However, Dr G had a very open and friendly manner about him which was instantly reassuring, we felt like equals from the offset so any tension we had felt beforehand quickly disappeared. He managed to hit my top two priorities on the head in pretty much the first sentence! He explained that he had been very interested in my unusual presentation and was keen to understand more, which is always difficult through email conversation. (not exactly a demanding list but surprisingly hard to find, especially among the surgical fraternity!)
Prior to the appointment I had submitted a series of questionnaires including; a CCI questionnaire, Oswestry Score, Kanofsky Scale , a basic analog pain scale (1-10 you know the drill) and a comprehensive medical and surgical history.
One of the questions was, "list your top 5 complaints in decreasing order of importance" now obviously, for me the number one slot goes to the Gastroparesis, followed closely by the headaches/migraine. This had really surprised him, he explained that he had never been approached by anyone with such severe gastric issues, especially as a primary concern over the headaches. I tried to explain as best I could that I have learnt to live with pain, pain is no longer a priority because I know it will always be there. I've had severe headaches for years but I've been told for so long that there's nothing wrong and no serious cause, that I stopped worrying about the severity and accepted them as part of my life (this is the short version obviously....more about this in part 3).
However, I strongly believe that ironically, the one thing that's keeping me alive will actually be what finishes me off and that's the TPN. I told him about my sepsis history and he instantly understood why that would be a priority to me.
So, having ironed out the small stuff we moved on to the scans. I had included my original radiology report with the scans so he could see what information I already had. Bearing this in mind, he went on to explain that he had re-calculated the measurements himself using the correct criteria (I will explain more about this in later blog) and the results were drastically different. He pulled up one of my images and said, "I'm sorry to have to show you this but you can see better than I can explain, yes?"
... However, Dr G had a very open and friendly manner about him which was instantly reassuring, we felt like equals from the offset so any tension we had felt beforehand quickly disappeared. He managed to hit my top two priorities on the head in pretty much the first sentence! He explained that he had been very interested in my unusual presentation and was keen to understand more, which is always difficult through email conversation. (not exactly a demanding list but surprisingly hard to find, especially among the surgical fraternity!)
Prior to the appointment I had submitted a series of questionnaires including; a CCI questionnaire, Oswestry Score, Kanofsky Scale , a basic analog pain scale (1-10 you know the drill) and a comprehensive medical and surgical history.
However, I strongly believe that ironically, the one thing that's keeping me alive will actually be what finishes me off and that's the TPN. I told him about my sepsis history and he instantly understood why that would be a priority to me.
So, having ironed out the small stuff we moved on to the scans. I had included my original radiology report with the scans so he could see what information I already had. Bearing this in mind, he went on to explain that he had re-calculated the measurements himself using the correct criteria (I will explain more about this in later blog) and the results were drastically different. He pulled up one of my images and said, "I'm sorry to have to show you this but you can see better than I can explain, yes?"
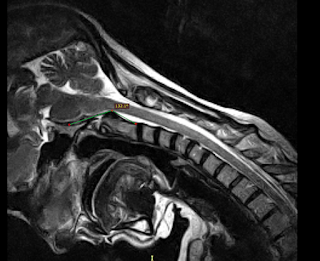 |
| Flexion Clivo-axial Angle 132.1º (Normal Range: 150º-180º) |
 |
| Neutral Clivo-axial angle 132.8 º (Normal Range:150º-180º) |
I don't think either of us expected to be able to see anything significant without a detailed explanation, but as he circled the area with his pen (where the angle is marked on this image) we both saw exactly what was going on. The room fell silent for a while, I don't think either of us knew what this really meant but we knew it wasn't good. I studied the Dr's face for a moment as I tried to grasp what I was seeing and saw the seriousness wash over his face. That expression you never want to see.
He explained that the dark area between the bone and where the angle is marked is a pannus formation (layer of fibrovascular/granulation tissue) which is a direct result of excessive movement of my Skull, C1 & C2 (the top two vertebrae). Effectively, instead of pivoting on the spine my head is sliding back and forth.
He went on to say that when he first saw the images, even without going over my symptoms he presumed that surgical fixation would be necessary due to the level of brainstem compression. He then explained that your head should not "slide" at all but there is a small tolerance of 1mm which they would deem abnormal but tolerable...anything more than that is a big problem. He then proceeded to demonstrate a calculation of my results (see table of measurements below) to determine precisely how much my head is sliding. I have to admit to not fully understanding this bit at the time but it wasn't 1mm... it was 4.3mm. These might sound like small numbers but even I can understand that 4 x greater than acceptable... is NOT acceptable!
Here is a list of my measurements for those who are interested:
Cervical spine flexion: 21º (Normal 12º)
Extension: 71º (Normal 32º)
Range of motion: >90º
Neutral CXA:132º
Flexion CXA:132º
Extension CXA:146º
CXA (Clivo-Axial Angle) Normal Range: 150º-180º
Neutral BDI: 11.6mm
Extension BDI: 12.1mm
Flexion BDI: 11.5mm
BDI (Basion Dens Interval) Normal: Less than 12mm
Neutral BAI: 8.6mm
Extension BAI: 3.6mm
Flexion BAI: 7.9mm
BAI (Basion Axial Interval) Normal: Less than 12mm
Translational BAI: 4.3mm (The "sliding" motion) Normal: 0-1mm
Neutral Grabb Oak: 9.6 mm (values greater than 9mm indicate ventral brainstem compression)
 |
| Grabb Oak Measurement |
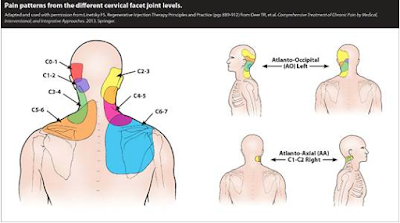
He then confirmed that my head is also over rotating when I look left and right which is causing subluxation (partial dislocation) of the facet joints.
Excessive rotation of the neck can be very dangerous in itself as the main vertebral artery runs down through C1 & C2, this image explains better than I can....
The vertebral artery is the main blood supply to the upper spinal chord, brainstem, cerebellum and posterior part of the brain so I'm sure I don't have to spell it out that damaging this could be catastrophic. Thankfully there is no impingement of this artery, but the excessive rotation is definitely playing its part in my overall symptoms, causing irritation and on it's own, carries significant risk.
Obviously all this information was way too much for us to fully understand at the time but neither of us was left in any doubt, we both fully understood what it meant underneath, regardless of the science.
If you're still reading... WELL DONE! I'm sorry to bore you with such detail but there was no other way to write this blog...believe me it's taken a few attempts! I think the crash course in neurology is enough for now so I will continue in Part #3 with the final outcome.


i'm so glad you finally have a an answer for some of your symptoms. i know how hard it is to live with a chronic illness. well done in taking control. NHS care for patients like us could be better. take care sam x
ReplyDeleteCan I have the doctors name (Dr. G)? I'm in the same boat and he is exactly what I need.
ReplyDelete